Why patients' voices must be at the forefront of driving Kenya's healthcare reforms

KNH has established both verbal and non-verbal communication channels, including social media platforms, to encourage patients and their families to provide feedback.
In 2022, Brian Kimani was diagnosed with a severe bladder condition that left him unable to control his urination. After several unsuccessful non-surgical treatments, he was admitted to a medical facility in Thika, where doctors inserted a silicone catheter into his bladder. The medical team assured him that the silicone catheter was the safest option, believed to reduce the risk of infection.
“The doctors told me the silicone wouldn’t cause infections,” Brian said. “But the pain started as soon as it was inserted—and it never really stopped.”
More To Read
- Only six in 10 Kenyan health facilities adequately equipped for quality care - report
- Report lays bare Kenya’s failing healthcare system
- Data gaps threaten Kenya’s health goals as key indicators on mental health, drugs go unmeasured
- Government proposes new health authority to regulate facilities, protect patients
- MPs slam Ministry of Health over SHA failures, demand urgent reforms
- Cabinet approves Bill to combat healthcare malpractice, enhance patient safety
Instead of providing relief, the catheter became a source of constant pain and discomfort. Brian explained that walking became extremely difficult, and urinating was agonising. Despite repeatedly raising concerns, he felt ignored by the medical staff.
“Every time I tried to speak up, they brushed me off,” he recalled. “They insisted that switching to another type of catheter would only lead to infections, so they refused to explore other options.”
The emotional strain of not being heard added to Brian’s physical suffering. He described the frustration of trying to explain the severe discomfort caused by the silicone catheter, only to be met with indifference.
“I kept telling them the silicone pipe wasn’t working for me,” he said. “It was painful and uncomfortable, but they treated my complaints like they didn’t matter.”
 Brian Kimani, who survived a serious bladder condition,n shares his story in an interview with The Eastleigh Voice at Kenyatta National Hospital during the Fourth Annual Patient and Family-Centred Care Symposium on April 30, 2025.(Photo: Justine Ondieki)
Brian Kimani, who survived a serious bladder condition,n shares his story in an interview with The Eastleigh Voice at Kenyatta National Hospital during the Fourth Annual Patient and Family-Centred Care Symposium on April 30, 2025.(Photo: Justine Ondieki)
As his condition worsened, Brian turned to Kenyatta National Hospital for help. There, for the first time, his concerns were taken seriously. Following a thorough evaluation, the medical team opted to perform another surgery to replace the silicone catheter with a Foley catheter.
“After months of living in pain, I finally had surgery at Kenyatta,” Brian said. “The cost was high, but a social worker stepped in and helped cover the expenses. That’s when I finally felt like someone cared and truly listened.”
While patient-centred care is often highlighted as a core objective in healthcare, it remains out of reach for many.
Ongoing systemic barriers—such as high costs, limited access, inequitable treatment, and poor communication—continue to undermine the quality of care. Many patients are still hesitant to give feedback, fearing they may be misunderstood, ignored, or even sidelined. At the same time, some healthcare providers perceive feedback as undue criticism, creating a lack of balance that ultimately leads to mistrust and, in some cases, further harm.
Ten years after receiving a life-saving kidney transplant at Kenyatta National Hospital (KNH), John Gikonyo reflects on the state of renal care in Kenya—and the many systemic gaps that still exist. "Many patients still don’t know their kidney health status," he explains, pointing to the urgent need for increased public awareness and education around kidney disease.
 The President of the Renal Society of Kenya John Gikonyo speaks to The Eastleigh Voice during the Fourth Annual Patient and Family-Centred Care Symposium at Kenyatta National Hospital on April 30, 2025.(Photo: Justine Ondieki)
The President of the Renal Society of Kenya John Gikonyo speaks to The Eastleigh Voice during the Fourth Annual Patient and Family-Centred Care Symposium at Kenyatta National Hospital on April 30, 2025.(Photo: Justine Ondieki)
While the government currently supports two dialysis sessions per week under the national renal programme—each costing approximately Sh10,600—there remain significant challenges in access and equity. Notably, some of the most crucial services, such as post-transplant care, are only available at KNH and Moi Teaching and Referral Hospital. Of the eight hospitals in the country that offer transplant services, only two are public, further limiting access for the majority of patients.
“Kidney treatment is very expensive in this country. Many of the services we now have weren’t just given—they came because we organised, advocated, and even went to KNH and SHA offices in person to demand change,” Gikonyo says.
Speaking during the 4th Annual Patient Care Symposium at Kenyatta National Hospital, Gikonyo emphasised the importance of open communication and timely feedback in improving healthcare delivery. He called on all stakeholders—healthcare providers, policymakers, and institutions—to prioritise active listening and genuine engagement with patients as a core part of quality care.
“I would like to encourage that, sometimes, when you visit a facility and find that a service is unavailable, it’s important to advocate for its inclusion. By doing so, we can ensure that everyone has access to the full benefits of the services they need”
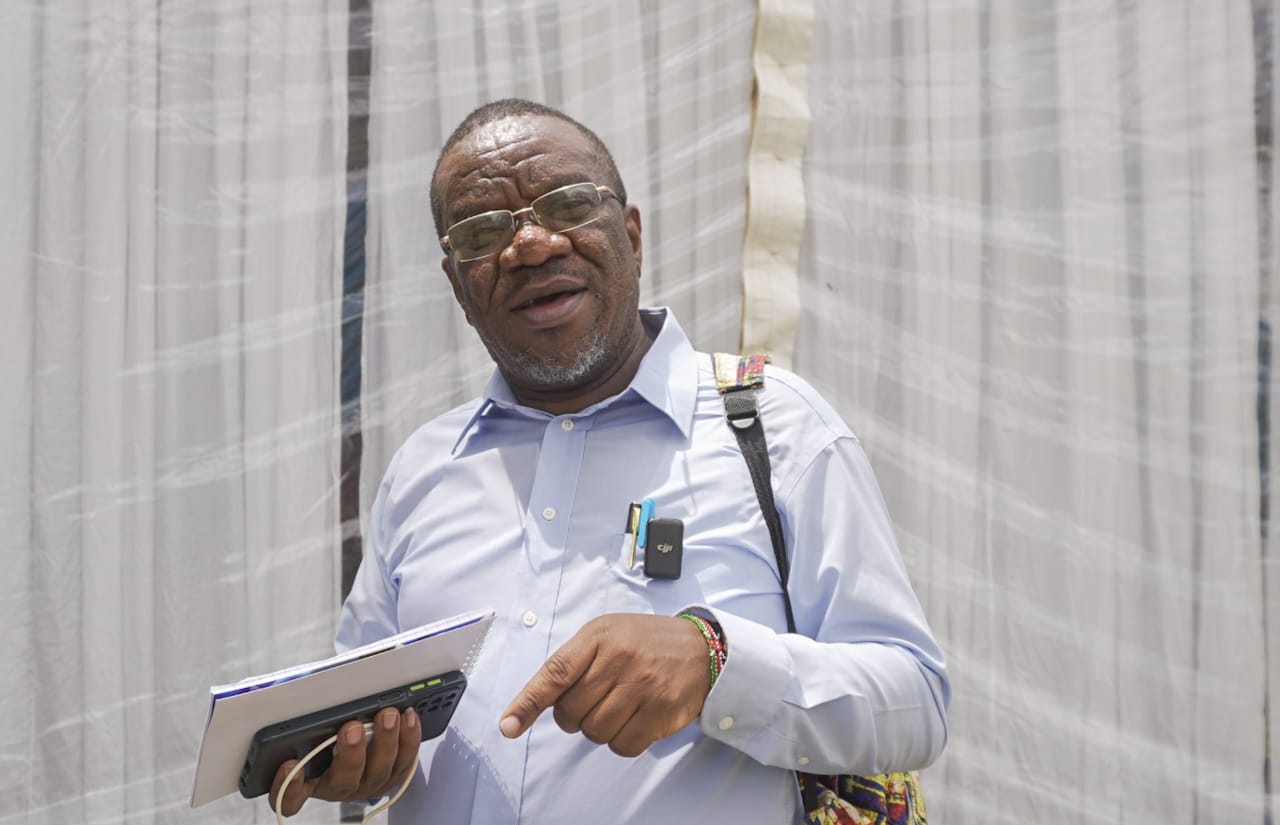 The President of the Renal Society of Kenya John Gikonyo speaks to The Eastleigh Voice during the Fourth Annual Patient and Family-Centred Care Symposium at Kenyatta National Hospital on April 30, 2025.(Photo: Justine Ondieki)
The President of the Renal Society of Kenya John Gikonyo speaks to The Eastleigh Voice during the Fourth Annual Patient and Family-Centred Care Symposium at Kenyatta National Hospital on April 30, 2025.(Photo: Justine Ondieki)
Speaking at the symposium, Dr William Siglai, representing the CEO of Kenyatta National Hospital (KNH), discussed the challenges of creating a healthcare environment that respects patients' needs while considering the financial constraints of today’s economy. “Financial limitations in today’s economy create significant barriers to accessing quality care,” Dr Siglai noted.
He stressed the importance of streamlining services and reducing costs without sacrificing quality. “It is crucial to ensure that healthcare remains affordable and patient-centred by prioritising cost-effective solutions that provide value while maintaining high standards of care,” he added. “Ultimately, high-quality care must be both accessible and affordable for everyone.”
Acknowledging the financial hurdles faced by many, Dr Siglai pointed out that too many individuals are unable to afford essential healthcare services.
 Dr William Siglai gives a statement on behalf of the Kenyatta National Hospital CEO during the Fourth Annual Patient and Family-Centred Care Symposium at Kenyatta National Hospital on April 30, 2025. (Photo: Justine Ondieki)
Dr William Siglai gives a statement on behalf of the Kenyatta National Hospital CEO during the Fourth Annual Patient and Family-Centred Care Symposium at Kenyatta National Hospital on April 30, 2025. (Photo: Justine Ondieki)
Kenyatta National Hospital has established both verbal and non-verbal communication channels, including social media platforms, to encourage patients and their families to provide feedback. This initiative aims to enhance the quality of services and address any concerns effectively.
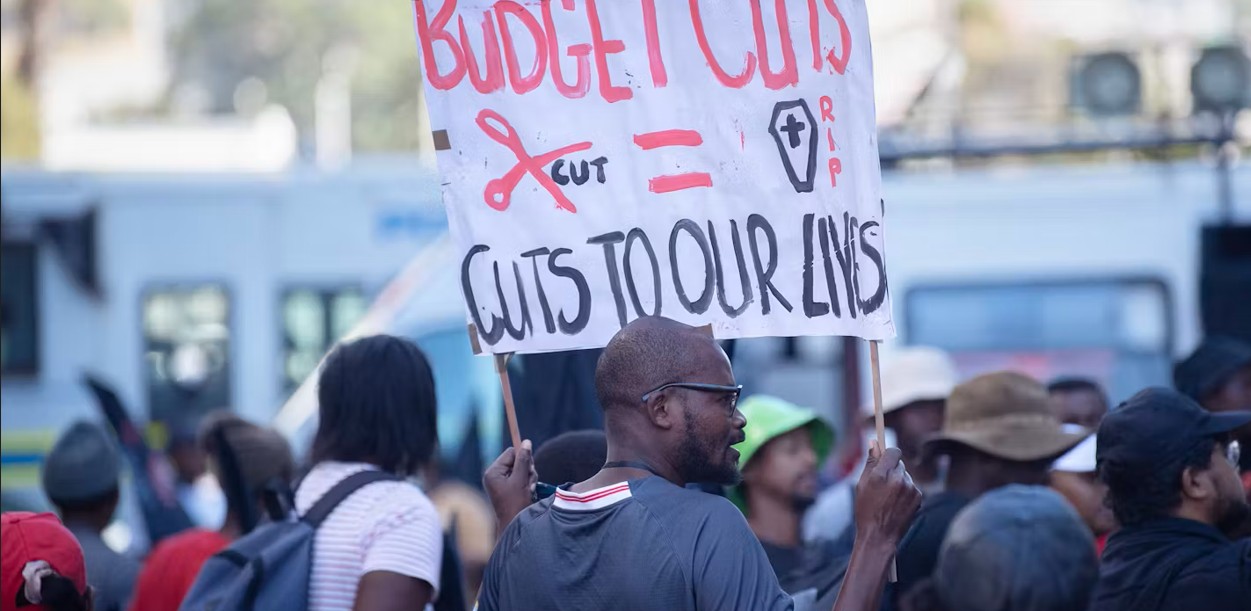
During the symposium, stakeholders raised serious concerns about the health sector, particularly the persistent gap between policy and implementation. One major issue is that although 15 per cent of the national budget should be allocated to healthcare, as per international commitments like the Abuja Declaration, this is rarely the case in practice.
Some groups feel disadvantaged while others appear more privileged, creating further inequality. Additionally, there’s a lack of clear leadership in some areas, leading to laxity and confusion over responsibilities.
 Participants who attended the Fourth Annual Patient and Family-Centred Care Symposium at Kenyatta National Hospital on April 30, 2025. (Photo: Justine Ondieki)
Participants who attended the Fourth Annual Patient and Family-Centred Care Symposium at Kenyatta National Hospital on April 30, 2025. (Photo: Justine Ondieki)
For instance, some citizens expect Members of Parliament to build hospitals—yet that is not their role. MPs are meant to provide oversight and push for policy changes, not take over the work of service delivery. This confusion of roles weakens service delivery and slows progress in healthcare.
Advocate groups noted that holding MPs and other leaders accountable is essential to build a culture of responsibility and follow-through. Without consistent public pressure, meaningful progress will remain out of reach.
When leaders and citizens don’t clearly understand or respect their roles, it leads to mismanagement and unmet needs. Advocacy and accountability are key to ensuring policies are not just written but implemented effectively.
Kenyans are encouraged to take an active role by demanding transparency, pushing for the full implementation of health policies, and holding leaders to account.
While the government continues to address various challenges in the health sector, patients are still raising concerns about the services they receive under the Social Health Insurance scheme. One key issue is the cost of outpatient services.
Although inpatient care is generally covered, many patients continue to incur out-of-pocket expenses for outpatient treatments, which remain largely uncovered for the general public. As a result, some individuals feel that the current health benefit package does not adequately meet their everyday healthcare needs.
Top Stories Today